How Is Sleep Apnea Diagnosed?
We diagnose sleep apnea based on your medical and family histories, a physical exam, and results from sleep studies.
Medical and Family Histories
Our practice will ask you and your family questions about how you sleep and how you function during the day. We will also ask you questions about to know how loudly and often you snore or make gasping or choking sounds during sleep. Often you're not aware of such symptoms and must ask a family member or bed partner to report them.
If you're a parent of a child who may have sleep apnea, tell your child's doctor about your child's signs and symptoms. Let your doctor know if anyone in your family has been diagnosed with sleep apnea or has had symptoms of the disorder.
Physical Exam
Dr. Yong will check your mouth, nose, and throat for extra or large tissues. The tonsils often are enlarged in children with sleep apnea. A physical exam and medical history may be all that's needed to diagnose sleep apnea in children.
Adults with the condition may have an enlarged uvula or soft palate. The uvula is the tissue that hangs from the middle of the back of your mouth. The soft palate is the roof of your mouth in the back of your throat.
Sleep Studies
A sleep study is the most accurate test for diagnosing sleep apnea. It captures what happens with your breathing while you sleep.
A sleep study is often done in a sleep center or sleep lab, which may be part of a hospital.
Diagnosis
Obstructive sleep apnea is diagnosed based on the number of apneas (cessation of breathing) or hypopneas (shallow breathing) observed per hour. These totals are combined into an index score called the apnea-hypopnea index (AHI). The AHI is the total number of apneas and hypopneas lasting 10 seconds or more, per hour.
The index is then used to create a diagnosis.
AHI or RDI |
Diagnosis |
More than 5 |
Mild sleep apnea |
More than 15 |
Moderate severe apnea |
More than 30 |
Severe sleep apnea |
Apneas, Hypopneas, and RERAs
Apneas, hypopneas, and RERAs (respiratory effort related arousals) are different types of sleep disturbances. The difference between them relates to the amount of reduction in airflow and blood oxygen saturation.
|
Reduction in airflow |
Reduction in blood oxygen saturation |
Length of time of disruption |
Accompanied by arousal? |
Apnea |
50% |
3%* |
10 seconds or more |
Yes |
Hypopnea |
30% |
4% |
10 seconds or more |
Yes |
RERA |
30% |
<4% |
10 seconds or more |
Yes |
* Some technicians will score apneas based on the 50% reduction in airflow alone.
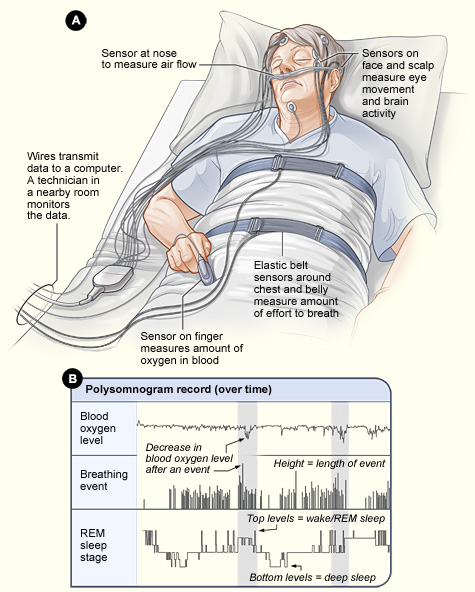
In order to accurately determine the frequency and severity of sleep disturbances, our practice will prescribe a sleep test, called a polysomnogram.
A polysomnogram (poly-SOM-no-gram), or PSG, is the most common study for diagnosing sleep apnea. This test records:
- Brain activity
- Eye movement and other muscle activity
- Breathing and heart rate
- How much air moves in and out of your lungs while you're sleeping
- The amount of oxygen in your blood
A PSG is painless. You will go to sleep as usual, except you will have sensors on your scalp, face, chest, limbs, and finger. The staff at our sleep center will use the sensors to check on you throughout the night.
The sleep study can be conducted in a sleep clinic or at home.
- Sleep clinic. In a sleep clinic, patients stay overnight and are hooked up to medical equipment that monitors all respiratory activity as well as brain activity.
- Home sleep test. The home sleep test is becoming more popular as it allows patients to sleep comfortably at home and many sleep doctors are advocating its use. The patient is connected to a device that monitors all respiratory activity including blood oxygen saturation, heart rate, sleep position, and breathing effort.
Our office reviews the results of your PSG to see whether you have sleep apnea and how severe it is. From there, we will use the results to plan your treatment.
Click here to see sample data from a sleep test.
Another sample:

This a 4 minute sample of a 7 hour sleep study that was performed on a patient. This shows what is checked during a sleep study and problem areas. This patient stopped breathing twice during the study for extended periods of time, this show is for a nearly 2 minutes and 30 seconds time span. Imagine being under water for over 2 mniutes, and the reaction that happens when comming out of the water to catch your breath and that will give you somewhat the idea of what this patient was experiencing.
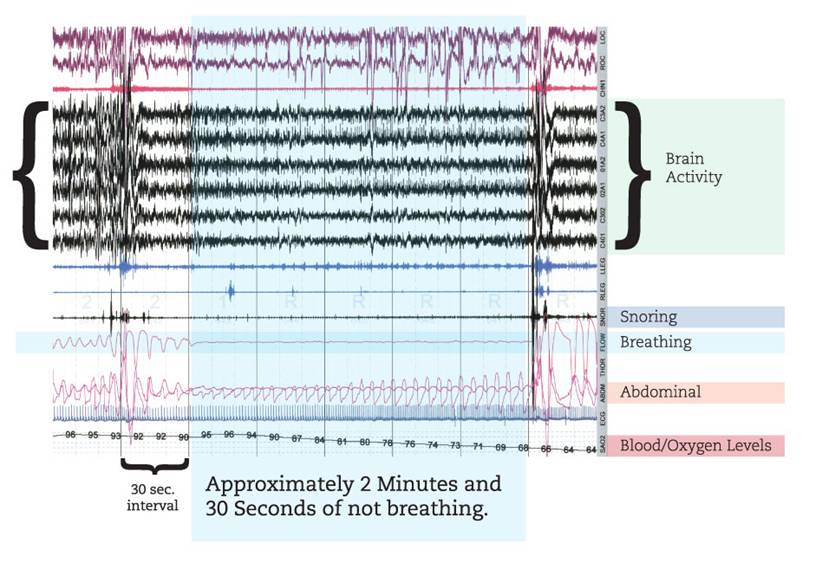
Breathing
 You can see where in the first minutes the patient is breathing, snores at about the 20 seconds and then stops breathing. They stop breathing for nearly 2 minutes and 30 seconds. At the 3:30 mark you can see their body startle, wake themselves up as theygasp to catch their breath.
You can see where in the first minutes the patient is breathing, snores at about the 20 seconds and then stops breathing. They stop breathing for nearly 2 minutes and 30 seconds. At the 3:30 mark you can see their body startle, wake themselves up as theygasp to catch their breath.
Blood/Oxygen Levels
The oxygen levels in the blood are normal at the beginning of the segment in the 90’s, but as the patient stops breathing, they drop to very low levels in the 60’s.
Abdominal
This measures the movement in the adominal section during your sleep. At the beginning, at the 30 second mark you can see movement associated with the snoring and then no movement for the time when the patient stops breathing and then the violent movement as they try to catch their breath.
Snoring
In this segment, their are two fairly abrupt snores. The first coming right before the patient stops breathing and then the violent one as they catch their breath at the 3:30 mark.
Brain Activity
The brain activity is measured during a sleep study. Here you can see the activity before, during and after the period where the patient wasn’t breathing.
If you’ve tried a variety of self-help sleep remedies without success, ask us about scheduling an appointment, especially if:
- Your main sleep problem is daytime sleepiness and self-help hasn’t improved your symptoms.
- You or your bed partner gasps, chokes, or stops breathing during sleep.
- You sometimes fall asleep at inappropriate times, such as while talking, walking, or eating.
UNATTENDED OVERNIGHT POLYSOMNOGRAPHY REPORT
PATIENT: |
xxxxxxxxxxxxx |
ACQ #: |
18 |
DOB: |
xxxxxx |
DATE OF STUDY: |
1/1/2011 |
REFERRING PHYSICIAN: |
Dr. Marjorie Yong, MD |
Tel: |
Fax: |
CONSULTING PHYSICIAN: |
Dr. Marjorie Yong, MD |
Tel: |
Fax: |
INDICATIONS: This is a 48 year old, (Gender: M) patient, 75 inches tall and weighing 195 lbs (BMI = 24.4), with a history of snoring, witnessed pauses in breathing, and daytime somnolence. An Epworth Sleepiness Scale score of 15 does indicate the presence of daytime somnolence. An overnight unattended polysomnogram is indicated to rule out the clinical impression of obstructive sleep apnea. |
PROCEDURE: An all-night unattended sleep study was performed in which the following medical parameters were recorded using a Philips Respironics model Alice PDx computerized polygraph measuring nasal airflow, oxygen saturation (pulse oximetry), chest & abdominal effort belts, sonogram (snoring) and body position. The raw data was manually reviewed and interpreted by Dr. Yong. The recording started on 1/9/2011 at 8:25:47 PM, and ended on 1/10/2011 at 4:37:47 AM. |
DEFINITIONS: |
CONCLUSION:
- sleep apnea with an Apnea Hypopnea Index (AHI) of 51.5 per hr.
- Severe sleep related oxygen desaturation.
- SaO2 nadir of 73% from a sleep baseline of 92%
- Severe respiratory related sleep fragmentation with a Respiratory Disturbance Index (RDI) of 55.6 per hr.
- Loud snoring was noted.
- Average duration of Hypopnea was 26.3 seconds.
- Maximum duration of Hypopnea was 51.5 seconds.
- Average duration of Apneas was 27.1 seconds.
- Maximum duration of Apneas was 52.0 seconds.
- In the morning questionnaire, the patient stated that he woke up 2 times for the restroom, did not remember any dreams, and that his sleep was the same as usual, including waking up at his usual time.